Weight Loss Cause Breakthrough Bleeding

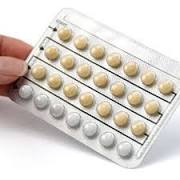
Bleeding on the Contraceptive Pill: What Causes It? Normally, when a woman takes the contraceptive pill she has a week off where she either doesn’t take anything or takes "dummy" pills that are inactive. During this time she will have her normal period. After these seven days, she resumes taking the pill. Sometimes, bleeding may occur at other times during the cycle while she is taking the pill. This is called "breakthrough bleeding". What Causes Breakthrough Bleeding? There are several reasons for spotting while on birth control: • If you have just started taking the pill you may bleed between periods because of the hormone disruption and your body getting used to the pill. It should stop after a few months and is not dangerous. It is usually milder than a regular period so you may need to wear pantyliners. If bleeding lasts longer than three months or is heavy, you may need to try a different pill or type of contraception. • If you forget to take pills, you are more likely to have irregular bleeding.

• If you smoke, you are more likely to have breakthrough bleeding because cigarettes have an anti-estrogenic effect that can disrupt cycles.
Moving Company Bratislava • Combined oral contraceptives that contain smaller amounts of active ingredients may cause irregular bleeding patterns more than pills with higher doses.
Patio Table Covers Elastic • Older generation pills don’t control bleeding as well as some of the newer pills.
House For Sale Cagayan De Oro City Philippines There are other causes of breakthrough bleeding which may not be related to the pill itself. Some medications interact with the pill. Check with your doctor that your medication is compatible with your contraception. • Sexually transmitted infections.

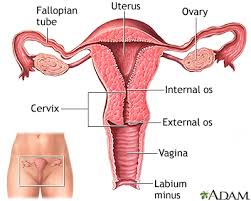
These may cause bleeding in between periods. The pill does not protect against sexually transmitted infections. • Other gynecological illnesses or cancer may cause bleeding. If the cause is known not to be due to the pill, the doctor may ask if he can do a Pap test to check for abnormal changes to the cervix or cervical cancer.Irregular periods are extremely common as the first sign of hormonal imbalance. Your body may just need extra support to return your menstrual cycle to its regular, healthy pattern. If your irregular periods continue, see your practitioner to find out what’s going on.Most of us have experienced irregular menstrual periods. These are usually due to temporary situations such as periods of extreme stress or new exercise routines. But it’s different if the irregularity continues with respect to length, frequency, spotting, or the “new” amount of bleeding during your period becomes a regular occurrence. At that point, you might start to feel worried or concerned, especially when you don’t know the cause.

Menstruation occurs every 21-35 days (average 28 days), with periods lasting from four to seven days, depending on the woman. As you can see, there’s a fair amount of variation and everyone is different. The entire menstrual process is orchestrated by hormonal signals and feedback loops between the brain and the ovaries. Most important is what’s normal for you.Irregular periods can be longer, shorter, heavier, or lighter than normal, and can include spotting or skipping days (or months). While there is no one set definition of an irregular period, you’re the best judge because you’re the one who will notice if there have been changes to your regular menstrual cycle pattern — which is really what “irregular” means.When your periods change suddenly, the most common cause is an imbalance in your hormones, especially estrogen and progesterone. Observing the pattern of irregularity and then asking yourself certain questions can help determine why your periods are off-kilter.Periods have become sporadic (oligomenorrhea) or disappeared for at least three months (amenorrhea).

Note: Ongoing irregular periods (including their absence) can be associated with bone loss.1) Perimenopause Perimenopause may account for about half of all irregular periods. In perimenopause, monthly ovulation becomes less reliable, eventually stopping completely, though the transition can sometimes last for years. Because ovaries are now responding less efficiently to pituitary hormones, periods and ovulation can become intermittent.Are you between 45 and 55?Has the number of days between periods increased?Have you been experiencing hot flashes, night sweats or other symptoms?2) Psychological stress Acute or chronic stress makes your body produce extra cortisol, a stress hormone. Because your body interprets stress as an emergency, it prioritizes ‘survival’ over reproductive function. Then estrogen and progesterone can become imbalanced, altering your periods until the stress eases.Have you been under more stress than usual? Do you have other stress symptoms?3) Physical stress Body stressors can have effects on the menstrual cycle similar to those of emotional stress.
Stress hormones hijack resources that would otherwise go toward producing sex hormones and normal cycles. Are you on a new fitness regimen?Did you recently start a strict diet?Did you recently lose a significant amount of weight?Have you suffered a recent illness?Did you quit smoking or change another long-time habit?4) Polycystic ovary syndrome PCOS affects 5-10% of premenopausal women. Continued lack of ovulation disrupts periods. They may be irregular, absent, or unusually heavy. In many cases, insulin resistance and signs of increased male hormones are present.Have you been experiencing acne or unusual hair growth?Do you have excess abdominal fat? (increases the risk)5) Prolactinoma High prolactin can cause periods to become irregular or stop altogether. Although high prolactin levels can be connected to low thyroid function, severe stress, pregnancy, and certain drugs, the most common cause is a benign pituitary tumor that produces the hormone.Have you noticed any nipple discharge?

Have you been trying to get pregnant without success?Do you have acne or unusual hair growth?Periods have been much heavier than normal (menorrhagia).Very heavy periods occur in 15-20% of otherwise-healthy women.Note: If your periods have been heavy for a while, ask your practitioner to test you for possible anemia.1) Perimenopause During perimenopause, progesterone levels can fall too low relative to estrogen. Then the uterine lining can thicken too much, so the period may be unusually heavy. (If your heavy periods are still regular, you’re probably still ovulating.)Are you between 45 and 55?2) Weight gain Fat tissue makes estrogen: the more you have, the greater the estrogen production. This can further thicken the uterine lining, resulting in heavier periods.Has your weight increased by more than 10-15 pounds within the past few months?3) Hypothyroidism Low thyroid function can cause heavier periods in many women. Hypothyroidism is involved in 20-45% of heavy periods.Have you been experiencing symptoms of hypothyroidism, such as sluggishness, puffiness, constipation, cold extremities, unexplained weight gain, fuzzy thinking, hair loss or depression?

You’re spotting between periods (metrorrhagia).Note: Sudden postmenopausal bleeding not caused by any of these should be checked by your healthcare practitioner.1) Menopause Vaginal tissues are thinner and more vulnerable to irritation when estrogen levels drop in menopause. Mild physical irritation causes tissues to bleed more easily.Any sudden postmenopausal bleeding that isn’t due to this cause should be checked immediately.Is the spotting occurring after sexual intercourse?Is intercourse physically uncomfortable?Do you have vaginal dryness?2) Abnormal pregnancy Fallopian-tube pregnancy or miscarriage can cause breakthrough bleeding in premenopausal women.Could you be pregnant?Do you have any history of miscarriage?3) Low-dose oral contraceptives, IUD, or postmenopausal hormone replacement therapy (HRT) Low-dose OCPs in premenopausal women and certain HRT in postmenopausal women may cause breakthrough bleeding. An IUD can sometimes cause spotting due to tissue irritation.Did you recently start taking birth control pills?

Do you have an IUD?Irregular periods can occur in conjunction with uterine fibroids, polyps, infections, malignancies, systemic disorders (e.g., liver or kidney disease, blood-clotting abnormalities), medication side effects, or recently-inserted IUDs. If your periods have been irregular for a while and none of these explanations seems to fit, consult your healthcare practitioner right away to schedule a physical exam and lab tests to rule out more serious issues.When it comes to balancing your hormones, you have more control than you may realize. After ruling out potentially serious issues, many doctors treat irregular periods with medication (e.g., birth control pills). These prescribed hormones fill in for your own hormones. Though this generally makes your periods run like clockwork, birth control pills can produce side effects without resolving the root source of the problem.If the abnormal bleeding you’re experiencing is related to lack of ovulation that results in estrogen ‘dominance,’ supplemental progesterone can help control heavy bleeding and/or regulate your period.
Several medicinal herbs, such as chasteberry, are also effective for regulating periods and boosting your own progesterone. Either of these approaches can help in perimenopause when progesterone is often low compared to estrogen. And if hypothyroidism is responsible for heavier periods, supplemental thyroid hormone can help.Three powerful ways to help restore regular periods are to make some simple adjustments to your diet:You may not be able to eliminate all the stressors in your life but you can achieve a healthy balance in your life with relaxation practices, regular exercise, plenty of sleep, and good, consistent nutrition. Your endocrine system is extremely sensitive to disruption, but it’s also resilient and responsive to healthy lifestyle and diet changes.Developing a more positive outlook can have a major impact as well — don’t discount the power of believing you can improve your health and well-being. Make sure you schedule regular checkups, including an annual physical exam, especially if your periods don’t get back to normal.